
The Link Between Insulin Resistance and Hormonal Imbalances in Women
The Hidden Connection Between Insulin Resistance and Women’s Hormones
Hormones are the body’s messengers. They control everything from energy and mood to fertility and metabolism.
But when one hormone system gets out of balance, it often affects others—especially in women.
One of the most common (yet often overlooked) connections is between insulin resistance and hormonal imbalances.
In this article, we’ll explore what insulin resistance is, how it affects women’s hormones,
its impact on conditions like PCOS, thyroid disorders, and menstrual irregularities, and natural ways to manage it.
What Is Insulin Resistance?
Insulin is a hormone made by the pancreas.
Its main job is to help glucose (sugar) move from the bloodstream into cells, where it can be used for energy.
In a healthy body: insulin works efficiently, and blood sugar stays in a safe range.
With insulin resistance: cells don’t respond well to insulin. The pancreas produces more insulin to “force” sugar into the cells.
Over time, this can lead to high insulin levels, high blood sugar, and eventually type 2 diabetes.
But even before diabetes develops, insulin resistance can disturb other hormone systems.
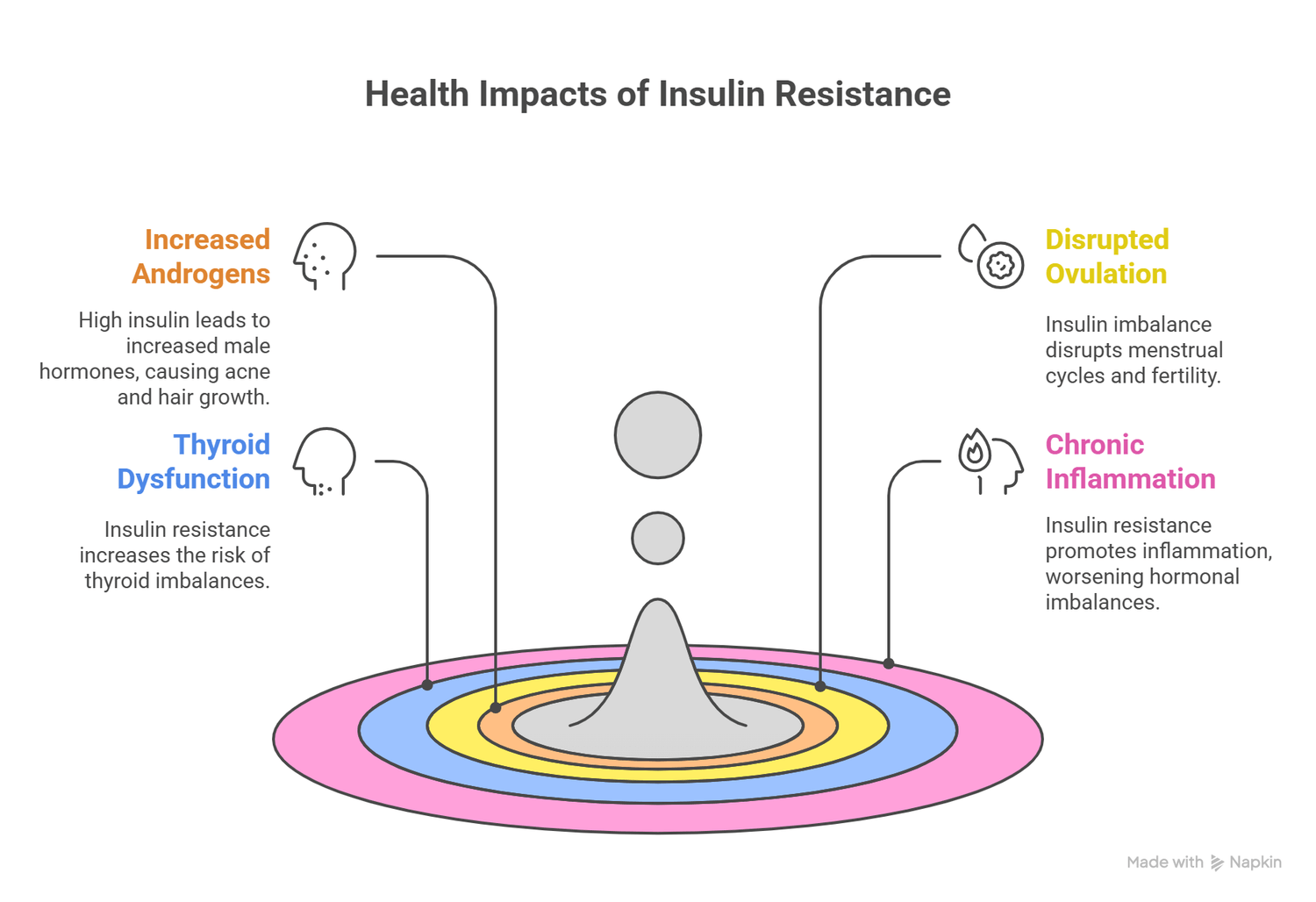
How Insulin Resistance Affects Women’s Hormones
Increases Androgens (Male Hormones)
High insulin stimulates the ovaries to produce more androgens like testosterone.
This can cause symptoms such as acne, oily skin, and excess hair growth.
Disrupts Ovulation
Too much insulin can disturb the delicate balance of estrogen and progesterone.
This often leads to irregular menstrual cycles and difficulty conceiving.
Impacts Thyroid Function
Research suggests that women with insulin resistance may also have a higher risk of thyroid imbalances, especially hypothyroidism.
Symptoms include fatigue, weight gain, and hair loss.
Insulin resistance promotes chronic low-grade inflammation,
which worsens hormonal imbalances and increases the risk of metabolic syndrome.
Conditions Linked to Insulin Resistance in Women
1. Polycystic Ovary Syndrome (PCOS)
PCOS is one of the most common hormonal disorders in women of reproductive age.
Up to 70% of women with PCOS have insulin resistance.
Symptoms: irregular periods, infertility, weight gain, acne, and hair growth on the face/body.
Insulin resistance worsens these symptoms by increasing androgen levels.
2. Menstrual Irregularities
High insulin levels disrupt normal ovulation, leading to missed or irregular cycles.
Some women may experience heavy bleeding, while others stop menstruating altogether.
3. Fertility Problems
Since ovulation is affected, many women with insulin resistance struggle to get pregnant.
It may also increase the risk of miscarriage.
Although the exact mechanism is still under study, insulin resistance and hypothyroidism often appear together.
This makes weight loss even harder and increases fatigue.

Symptoms of Insulin Resistance in Women
You might not know you have insulin resistance because symptoms are subtle at first.
Some warning signs include:
Constant fatigue and low energy
Cravings for sugar or carbs
Difficulty losing weight (especially around the belly)
Dark patches of skin (acanthosis nigricans) on the neck or armpits
Irregular periods
Acne or unwanted facial/body hair
Hair thinning
If several of these symptoms sound familiar, it’s worth discussing with a doctor and getting blood tests for glucose, insulin, and other hormones.
How to Naturally Improve Insulin Sensitivity
The good news is that insulin resistance is reversible, especially when detected early.
Lifestyle changes play a key role.
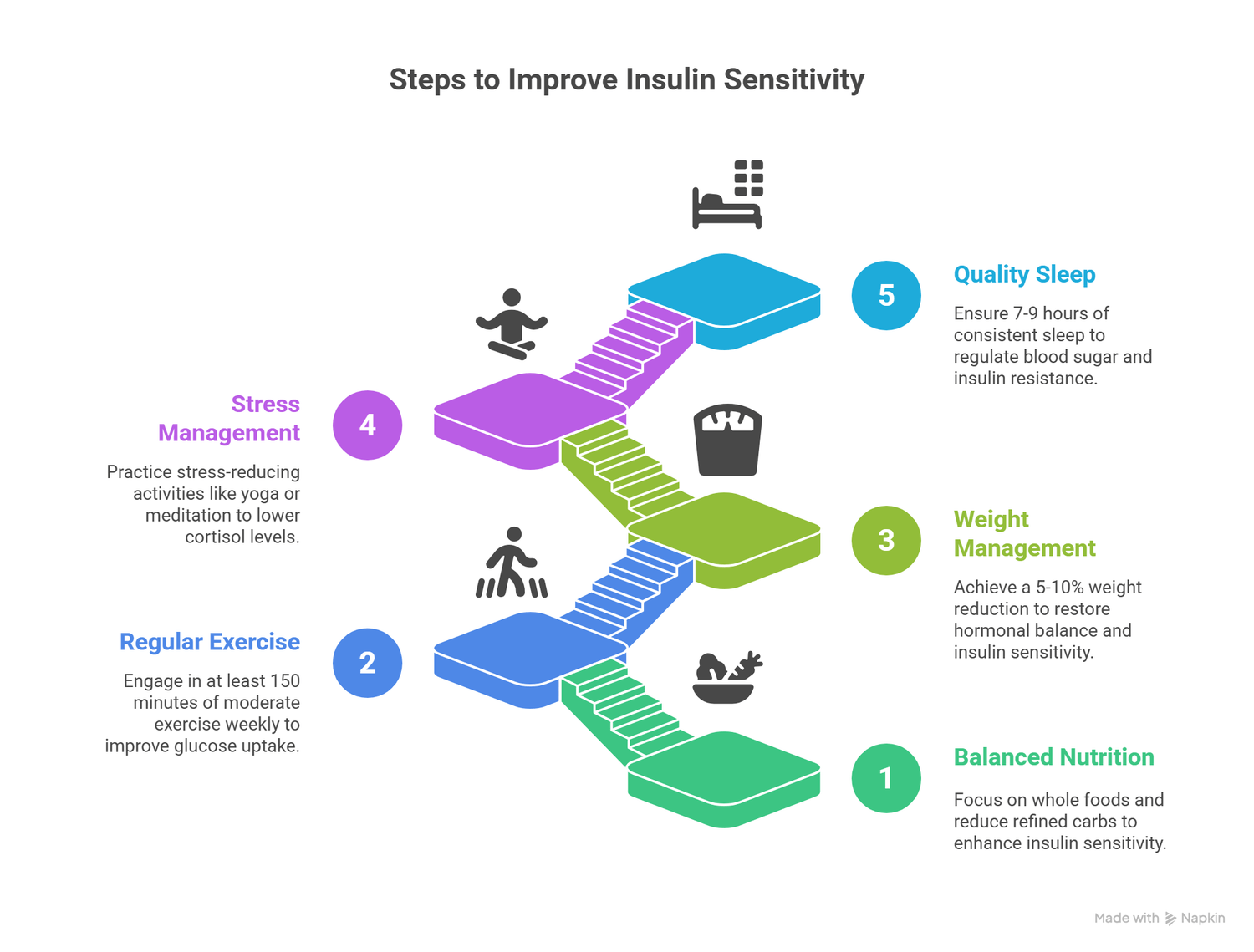
1. Balanced Nutrition
Focus on whole foods: vegetables, fruits, lean proteins, whole grains, and healthy fats.
Reduce refined carbs (white bread, sweets, sugary drinks).
Add foods that improve insulin sensitivity:
Magnesium-rich foods (spinach, almonds, pumpkin seeds)
Omega-3 fatty acids (salmon, chia seeds, walnuts)
Cinnamon and turmeric (natural insulin-sensitizers)
2. Regular Exercise
Aim for at least 150 minutes per week of moderate exercise like walking, cycling, or swimming.
Strength training helps build muscle, which improves glucose uptake.
3. Weight Management
Even a 5–10% reduction in body weight can significantly improve insulin sensitivity and restore hormonal balance.
4. Stress Management
Chronic stress increases cortisol, which worsens insulin resistance.
Practices like yoga, meditation, deep breathing, or simply walking outdoors can lower stress.
5. Quality Sleep
Poor sleep raises blood sugar and insulin resistance. Aim for 7–9 hours per night with a consistent sleep routine.
Medical Support
While lifestyle is the foundation, some women may also need medical help.
Doctors may prescribe metformin, a medication that improves insulin sensitivity.
In PCOS, hormone-balancing therapies may also be considered.
Always consult with a healthcare professional before starting any medication or supplement.
Key Takeaways
Insulin resistance is more than a blood sugar problem—it directly impacts women’s hormones.
It is strongly linked to PCOS, menstrual issues, thyroid disorders, and fertility problems.
Early recognition of symptoms such as fatigue, cravings, acne, and irregular periods can help women seek timely treatment.
Nutrition, exercise, stress management, and quality sleep are powerful natural tools to reverse insulin resistance and restore balance.
Conclusion
The connection between insulin resistance and hormonal imbalance in women is undeniable.
By understanding the link and making proactive changes, women can not only reduce the risk of diabetes but also restore healthy cycles, improve fertility, and feel more energetic every day.
Taking charge of insulin health is, in many ways, taking charge of hormonal health and overall well-being.
